In our meeting, we reviewed Alex Thompson’s BPMH and identified key strategies to ensure he feels safe and supported during the process, as well as potential discrepancies that could impact patient safety.
Trauma-Informed Strategies for Interviewing Alex Thompson
To create a comfortable and inclusive environment, we discussed the following approaches:
- Professional Introduction – Stating our name, role, and intentions to establish trust.
- Offering Support Before Beginning – Asking if he needs anything to feel more comfortable.
- Respecting His Identity – Confirming his preferred name and pronouns before proceeding and throughout our conversation.
- Providing Alternative Safe Spaces – If he expresses discomfort, offering a private space for discussion.
- Open-Ended Questions – Encouraging feedback from Alex rather than simple yes/no responses.
- Partner Involvement – Since his partner helps with his medication routine, asking if he would like them to join the conversation for added support.
- Using Simple, Clear Language – Avoiding complex medical terms (e.g., saying “high blood pressure” instead of “hypertension”).
- Demonstrating Active Listening – Engaging with his responses, being patient, and validating his concerns.
- Displaying LGBTQIA2S+ Support – Wearing a symbol of inclusivity (e.g., a wearable pin on our clothing, or pen, or logo on our shirt) to reinforce that he is in a safe space.
Identify potential discrepancies, missing details, or unsafe details in the BPMH and explain how they could impact patient safety.
Medication Safety Concerns in BPMH
We also identified missing details, discrepancies, and potential safety risks in the BPMH:
- Medication Allergies – The BPMH lists allergies but what is missing is his reaction severity details, which could impact safe prescribing.
- Weight and Height Missing – These details are necessary for dosing calculations, particularly for lisinopril and testosterone therapy. (often times during hospital stay a patients meds require weight or BSA)
- Limited Medication Verification Sources – The BPMH was only confirmed with Alex himself, but his anxiety and PTSD may affect recall, making pharmacy and caregiver verification important.
- Community Pharmacy Confirmation Needed – Since he fills prescriptions at multiple pharmacies, contacting his pharmacies ensures medication adherence and safety.
- Time Format Standardization – Documenting medication administration times using a 24-hour format for accuracy.
- When writing the date of BPMH, include the full date, day/month/year.
- Unclear Testosterone Therapy Details – The BPMH lacks precise timing information on testosterone injections, which could impact hormonal stability and side effects. Confirmation from who is injecting his testosterone for an accurate BPMH is important.
- Lisinopril Dosing Unclear – No measurement unit (mg?, g?, mL?) listed, increasing the risk of incorrect dosing.
Final Takeaways
Our discussion emphasized that by applying trauma-informed practices, ensuring comprehensive medication verification, and improving documentation clarity, we can enhance patient safety and create a trusting, supportive healthcare experience for Alex. In our discussion, we found an infographic that we found helpful and it is included here to help with future interviews. We also used the following references which helped guide us with how we would address not only Alex, but also in our future encounters with patients when performing best possible medication history interviews.
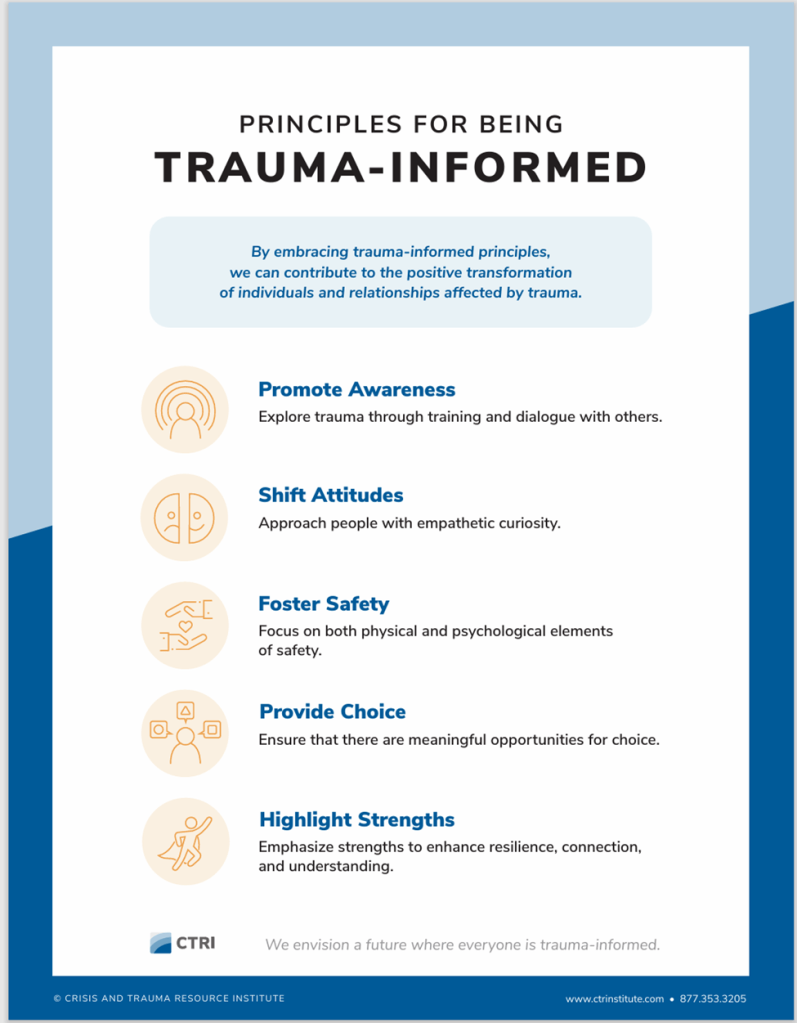
(CTRI, n.d.)
References:
CTRI. (n.d.) Principles for being trauma-informed. Crisis and Trauma Resource Institute. Retrieved from.Trauma Informed Care Poster v3
ISMP Canada Safety Bulletin. (March 26, 2024) Safe spaces: psychological safety for patients. (Volume 24. Issue 3). Institute for Safe Medication Practices Canada. Retrieved from. ISMPCSB2024-i3-Psychological-Safety
ISMP Canada. (n.d.) Best possible medication history interview guide. Retrieved from. BPMH-Interview-Guide
Leave a comment